26
Jan
21
01-4532698
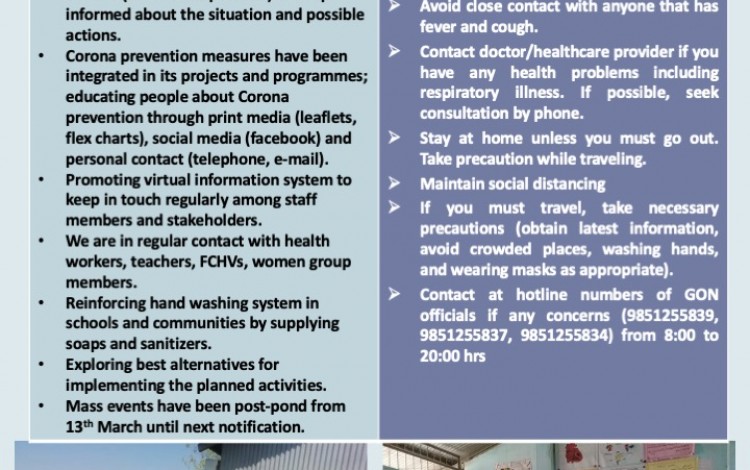
Green Tara Nepal, a non-governmental, apolitical and non-profit making organization, established in 2007. It works in research, publications, advocacy, training and social mobilization in a holistic community development approach.
Green Tara Nepal works in collaboration and cooperation with community people, CBOs, NGOs, civil societies and, external development partners at national and international level and. It works in close coordination with the government sector at federal, provincial, district and local level.
Contribute to improve maternal, newborn and adolescent health (MNAH) Background: In Nepal, despite a lot of progress has been made during the last decade in terms of decrease of mortality rates for women and new-borns and coverage of matern...
View ProjectLearning Champions Despite Pandemic: Strong Girls II (2022-2026) 1.0 Background: Strong Girls Project (Sept. 2018 – Apr. 2022) focused on improving the quality of education in the targeted areas among Dalit and marginalized girls and...
View ProjectSchool and Community Health Promotion Project, 2023-2028 Summary of the Project 1.0 Background: Kids at School in Nepal (KASIN), is a Charity organisation working in Nepal since 2004, with the vision that all children have the right to a dece...
View ProjectPromotion of Child, Adolescent and Maternal Health Promotion Project- Dolakha (DHP) (2022-2025) Background: ChildAid Network (CAN) –a Germany based non-government organization has been supporting rural communities in Nepal for improving health,...
View ProjectImproving Access to Maternal and Child Health Care and Family Planning by Strengthening the Health System and Promoting Health in Rural Areas of Nepal PROJECT BRIEF Background In Nepal, maternal, neonatal and child health (MNH...
View ProjectResearch: Promoting evidence-based interventions and policy advocacy GTN promotes evidence-based practices and research in coordination with academia and experts. GTNs experiences in managing research projects are summarised below:...
View ProjectDignity for Women - Ending Chhaupadi: Safe menstruation instead of stigmatisation and exclusion and access to reproductive health in Western Nepal PROJECT BRIEF Description The Dignity for Women Project launched in September 2021 and is projected to...
View Projectmembers
projects

Our team

CHAIRPERSON

COUNTRY DIRECTOR

TREASURER

What people says about us.
Green Tara Nepal, in collaboration with Green T...

Our awareness blog

26
Jan
21
14
Mar
20

We are associated with following partners: